/ Nov 05, 2025
Trending
Dan Carter, ND
Male hormone restoration implies that all hormones that decline with age or suboptimal metabolism should be restored to levels consistent with optimal physiologic function. Hormone restoration includes all major hormones that affect biologic function, including testosterone, dehydroepiandrosterone (DHEA), thyroid, and melatonin. Growth hormone is useful for many individuals as they age, but its expense eliminates it from consideration for most patients; hence, it will not be included in this discussion. What will be covered herein are some of the lesser-known benefits of hormone restoration, emphasizing testosterone.
Replacement:
1: the action or process of replacing: the state of being replaced.
2: one that replaces another especially in a job or function
Restoration: 1: an act of restoring or the condition of being restored: as a bringing back to a former position or condition. 2: something that is restored; especially: a representation or reconstruction of the original form
Merriam-Webster Online
When used in the context of improving a man’s health, hormone restoration is the better term. What happens during aging that can be related to hormone decline? Alterations include decreased capacity for cellular protein synthesis, decline in immune function, loss of muscle strength and function, fatigue, increased body fat, decreased bone density, erectile dysfunction, decreased libido, depressed mood, and more “age related” illness.1 These changes lead to age-related disability, including less strength and endurance, muscle atrophy, impaired mobility, less physical and mental energy, and osteoarthritis. The downward cycle resulting from these disabilities results in falls, fractures, loss of independence, and poor quality of life. Hormone restoration can delay the effects of aging and allow for a longer period in a functional and healthier state. This is an important aspect of preventive medicine.
Testosterone
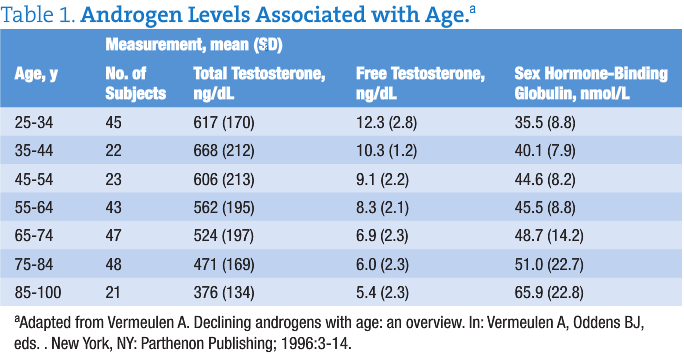
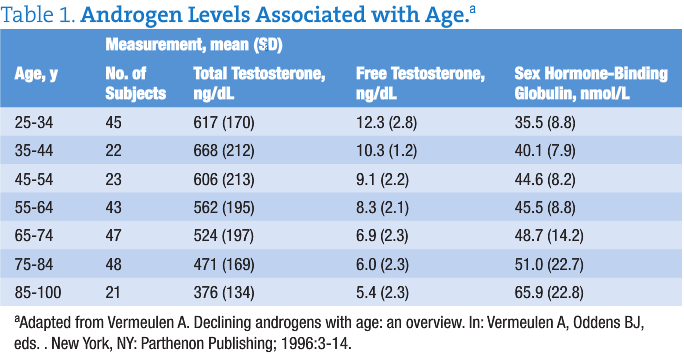
The following quotation is from WebMD: “Testosterone levels decline steadily after age 40. The decline is relatively small, at an average rate of about 1% to 2% percent [sic] per year. By middle age and older, virtually all men experience some decline in testosterone — but only a small percentage of aging men have levels far below those considered normal for their age” (Hoffman M. Low testosterone explained: how do you know when levels are too low? http://men.webmd.com/features/low-testosterone-explained-how-do-you-know-when-levels-are-too-low). Table 1 gives androgen levels among subjects by age group. What the WebMD quotation implies is that testosterone should be adjusted to an age-normal level; more benefit is realized when testosterone is replaced to a level consistent with highest metabolic function (ie, the free testosterone level seen in the group aged 25-34 years). Blood testosterone is monitored by periodic serum concentration testing to ensure a safe and therapeutic level.
Risks and Contraindications of Testosterone Therapy
Histories of prostate cancer or breast cancer are absolute contraindications for testosterone therapy. Testosterone can make both of these hormone-sensitive cancers grow more rapidly. Possible Adverse Effects of Testosterone Therapy Following is a list of possible adverse effects of testosterone restoration:
1. Fluid retention. Some healthy older men have shown problems with fluid retention, leading to ankle or leg swelling, worse high blood pressure, and possibly congestive heart failure, according to older data. In a 2005 study of extracellular water in hypopituitary men, no patients reported adverse effects, and no clinical symptoms or signs associated with excess fluid retention were observed during treatment with the doses and regimen used for growth hormone, testosterone, or their combination.2
2. Liver toxic effects. To date, there are no reports of liver toxic effects from transdermal testosterone therapy. Oral testosterone therapy can cause significant liver problems.
3. Decreased fertility. Exogenous testosterone shuts down sperm production significantly or completely in almost all men, and this can be a temporary or permanent effect. It is recommended that men delay testosterone therapy until they have finished having children.
4. Sleep apnea. Increased testosterone levels may exacerbate preexisting sleep apnea. However, a 36-month trial of testosterone therapy in older men demonstrated no effect of treatment on apneic episodes.
5. Tender breasts and gynecomastia. This may occur in older men receiving testosterone therapy due to the conversion of testosterone to estrogen. Breast tissue is estrogen sensitive, and this adverse effect can be eliminated by decreasing the dosage or by prescribing an aromatase inhibitor.
6. Polycythemia. Men who develop polycythemia can lower their testosterone dosage or donate blood to decrease their blood cell mass. It is advisable to check hematocrit readings yearly.3 [Physicians commonly confuse malignant polycythemia vera with erythrocytosis. Testosterone increases erythropoeitin production by the kidneys. This is the same process that causes individuals who live at high altitudes to have increased red blood cell counts. Erythrocytosis does not need to be treated, as it is a benign condition].
7. Prostatic hyperplasia. Hyperplasia may be benign (benign prostatic hypertrophy), with its attendant problems with urination. Testosterone may promote the growth of cancerous prostate cells.
For carefully screened patients, the benefits of testosterone therapy are greater than the risks.
Low free testosterone levels are an independent risk factor for cardiovascular disease. Older men with low free testosterone levels and low high-density lipoprotein cholesterol concentrations showed more severe coronary artery blockage than those evaluated by predictors, including blood pressure, elevated cholesterol, diabetes mellitus, smoking, and body mass index.4
Possible Cardioprotective Activities of Testosterone Therapy
Testosterone exhibits a number of possible cardioprotective activities. Significant examples include the following:
• Reduces serum levels of the proinflammatory cytokines interleukin (IL) 1β and tumor necrosis factor
• Increases levels of the anti-inflammatory cytokine IL-10
• Reduces vascular cell adhesion molecule 1 expression in aortic endothelial cells
• Promotes vascular smooth muscle and endothelial cell proliferation
• Induces vasodilatation and improves vascular reactivity, to reduce serum levels of the prothrombotic factors plasminogen activator inhibitor 1 and fibrinogen
• Lowers low-density lipoprotein cholesterol concentrations
• Improves insulin sensitivity
• Reduces body mass index and visceral fat mass
Taken together, the actions of testosterone confer cardiovascular benefit, as testosterone therapy reduced atheroma formation in cholesterol-fed animal models and decreased myocardial ischemia in men with coronary heart disease.5 Insulin resistance occurs in chronic heart failure (CHF) and implies a worse prognosis.6 Investigations in men without CHF showed that physiologic testosterone therapy improves insulin sensitivity. This 2007 study6 showed that testosterone restoration improves fasting insulin sensitivity in men with CHF and increases lean body mass. The data suggest a beneficial effect of testosterone on an important metabolic component of CHF. Low testosterone levels predict cardiovascular events such as stroke and transient ischemic attack in older men and are associated with higher cardiovascular and overall mortality.7
Other Considerations Regarding Testosterone Therapy
Men with chronic medical or psychological illnesses should have their testosterone level measured, especially when sexual dysfunction symptoms or signs are present (eg, erectile dysfunction).8 Depression and hypogonadism are also associated with erectile dysfunction. Physicians should evaluate testosterone measurements in all men with high depression symptom scores.9 Metabolic syndrome and insulin resistance are also significantly associated with low testosterone levels in older men. Men with metabolic syndrome should not only have cardiovascular risks evaluated but also have testosterone levels assessed.10
Historically, visceral obesity, metabolic syndrome, diabetes mellitus, cardiovascular disease, and erectile dysfunction were viewed as independent conditions affecting the aging man. It is becoming recognized that hypogonadism is a common third denominator of a triad that includes erectile dysfunction and metabolic syndrome.11 Dehydroepiandrosterone
Dehydroepiandrosterone is the most common corticosteroid hormone in the body and is produced mainly by the adrenal glands. Dehydroepiandrosterone is derived from pregnenolone, which is metabolized from cholesterol. Dehydroepiandrosterone can be converted into other sex hormones, including testosterone and the estrogens, although this is more common in women.12 By age 60 years, DHEA levels are only about 5% to 15% of what they were at their peak at age 20 years and can be considered a biomarker of aging.13 Dehydroepiandrosterone has been reported to have beneficial effects for patients with diabetes, senile dementia, obesity, immunosuppression, and autoimmune conditions. It also shows promise in cancer prevention (by increasing natural killer cells), stress-induced diseases, aging, and heart disease.14,15
A suitable daily dose of dehydroepiandrosterone in aging men is 50 mg, as it leads to serum DHEA sulfate concentrations similar to those measured in young healthy adults.16 Serum testosterone and dihydrotestosterone levels remained unchanged after administration of 50 mg of dehydroepiandrosterone. However, 17-beta estradiol and estrone levels significantly increased to concentrations still within the upper normal range for men. A dehydroepiandrosterone-induced increase in estrogens may contribute to beneficial effects of DHEA in men.
Thyroid Hormone
Low free thyroid hormone levels can occur as a consequence of aging, despite normal thyrotropin levels.17 Certain prescription drugs can also effect total thyroxine (T4) metabolism, including carbamazepine, phenytoin, rifampin, and phenobarbital. Additional drugs such as amiodarone and lithium can affect thyroid function in other ways. Thyroid disease can also manifest with symptoms derived from the most diseased nonthyroid system in the patient.18 In the presence of normal thyrotropin values, patients with hypothyroid symptoms can benefit from having free T4 and total triiodothyronine values determined.
Melatonin
A common belief is that “melatonin levels slowly drop with age and older adults make very small amounts of it or none at all.” Older research supports the decrease in melatonin with aging, whereas newer research refutes it.19 Sleep disturbances become more common with aging, and sufficient restorative sleep is important for overall health. Melatonin also inhibits the growth of several types of cancer cells. Melatonin limits human prostate cancer cell growth by a mechanism that affects the regulation of androgen receptor function; other mechanisms may be involved.20,21 The physiologic surge of melatonin at night can be considered a “natural restraint” on tumor initiation, promotion, and progression.22 Although declining melatonin production during the aging process is not thoroughly elucidated, many patients experience better sleep with sufficient dosing. Melatonin dosage is based on the amount that gives restful sleep without morning grogginess.
Pre–Hormone Restoration Therapy Examinations
The following clinical and laboratory examinations should be considered a minimum workup before administering hormone restoration therapy:
• Complete blood cell count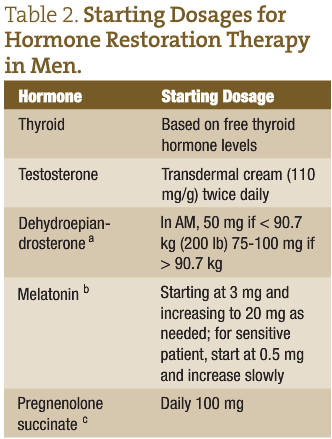
• Comprehensive metabolic panel
• Prostate-specific antigen test
• Digital rectal examination
• Testicular examination
A thorough medical history is also mandated.
Starting Dosages for Hormone Restoration Therapy
Table 2 gives starting dosages for hormone restoration therapy in men.
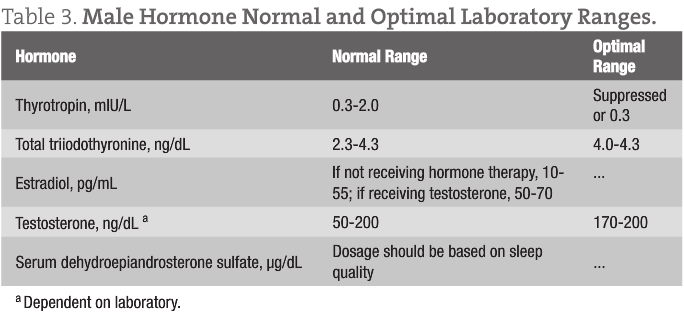
Testing of Hormone Levels
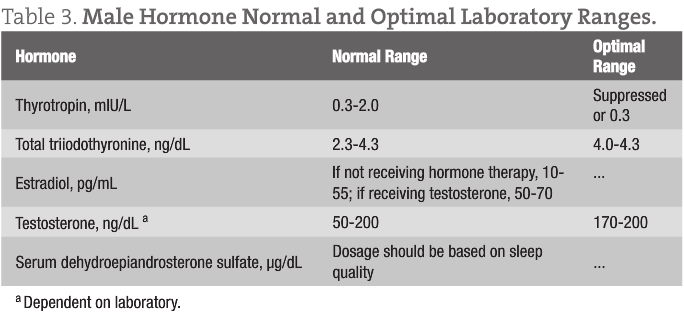
Hormone levels should be determined 1 month after initiation of hormone restoration therapy. Blood serum levels are the preferred testing method; blood should be drawn 5 hours after the morning dose of hormone. Testing applies to thyroid hormone, testosterone, and DHEA sulfate levels. Estradiol is not normally tested in men; the value is included for reference in Table 3. Melatonin level is not tested. Once a therapeutic hormone level is reached, testing is normally performed once a year. Optimal values are selected using the top end of the male normal range.
In conclusion, a carefully designed and monitored hormone restoration program improves the quality of life in aging men. For men exhibiting central obesity, often in conjunction with metabolic syndrome, it is important that they receive dietary counseling to help reduce visceral adiposity. Aromatase enzyme levels are increased in patients with visceral fat and high insulin levels; high aromatase levels convert too much testosterone to estrogen, leading to more abdominal and pectoral fat and gynecomastia. Visceral adiposity normally responds well to a diet that improves insulin sensitivity by restricting carbohydrate consumption, while supplying sufficient protein and fat.
Dan Carter, ND, graduated from National College of Naturopathic Medicine (NCNM) and completed a 2-year family practice resi-dency at the college. He was appointed to a full-time faculty position in 1997 and served as a core faculty member through 2003.He is a co-founder of IV Nutritional Therapy for Physicians, teaching intravenous thera-py workshops since 1991. These workshops provide com-plete training to physicians internationally for the safe and effective use of intravenous nutrient therapies. He has been in private practice in Bozeman, Montana since 2004. His practice focuses on the nutritional improvement of health, weight loss, hormone restoration for men and women, and IV nutrient therapy. Dr Carter’s websites can be accessed at www.alpinephysicians.com and www.bznwtmgt.com.
SIDEBAR • Meta-analysis indicates testosterone is not associated with increased risk of cancer • Testosterone does not cause cancer23 • Testosterone increases the growth of prostate cancer if present • Prostate cancer is most prevalent when testosterone levels are low
References 1. Winters SJ. Current status of testosterone replacement therapy in men. Arch Fam Med. 1999;8(3):257-263. 2. Johannsson G, Gibney J, Wolthers T, Leung KC, Ho KK. Independent and combined effects of testosterone and growth hormone on extracellular water in hypopituitary men. J Clin Endocrinol Metab. 2005;90(7):3989-3994. 3. Haijar R, Kaiser F, Morley J. Outcomes of long-term testosterone replacement in older hypogonadal males: a retrospective analysis. Clin Endocrinol Metab. 1997;82(11):3792-3796. 4. Phillips G, Pinkernell B, Jin T. Are major risk factors for mycocardial infarction the major predictors of degree of coronary artery disease in men? Metabolism. 2004;53(3):324-329. 5. Jones RD, Nettleship JE, Kapoor D, Jones HT, Channer KS. Testosterone and atherosclerosis in aging men: purported association and clinical implications. Am J Cardiovasc Drugs: 2005;5(3):141-154. 6. Malkin CJ, Jones TH, Channer KS. The effect of testosterone on insulin sensitivity in men with heart failure. Eur J Heart Fail. 2007;9(1):44-50. 7. Yeap B. Androgens and cardiovascular disease. Curr Opin Endocrinol Diabetes Obes. 2010;17(3):269-276. 8. Guay A, Seftel A, Traish A. Hypogonadism in men with erectile dysfunction may be related to a host of chronic diseases. Int J Impot Res. 2010;22(1):9-19. 9. Makhlouf, A, Mohamed, M, Seftel A, Niederberger C. Hypogonadism is associated with overt depression symptoms in men with erectile dysfunction. Int J Impot Res. 2008;20(2):157-161. 10. Guay A, Jacobson J. The relationship between testosterone levels, the metabolic syndrome (by two criteria), and insulin resistance in a population of men with organic erectile dysfunction. J Sex Med. 2007;4(4, pt 1):1046-1055. 11. Ahabsigh R. The triad of erectile dysfunction, hypogonadism and the metabolic syndrome. Int J Clin Pract. 2008;62(5):791-798. 12. Morales AJ, Nolan JJ, Nelson JC, Yen SS. Effects of replacement dose of dehydroepiandrosterone in men and women of advancing age [published correction appears in J Clin Endocrinol Metab. 1995;80(9):2799]. J Clin Endocrinol Metab. 1994;78(6):1360-1367. 13. Ebeling P, Koivisto VA. Physiological importance of dehydroepiandrosterone. Lancet. 1994;343(8911):1479-1481. 14. Rudman D, Shetty KR, Mattson DE. Plasma dehydroepiandrosterone sulfate in nursing home men. J Ann Geriatr Soc. 1990;38(4):421-427. 15. Kalimi M, Shafagoj Y, Loria R, Padgett D, Regelson W. Anti-glucocorticoid effects of dehydroepiandrosterone (DHEA). Mol Cell Biochem. 1994;131(2):99-104. 16. Arlt W, Haas J, Callies F, et al. Biotransformation of oral dehydroepiandrosterone in elderly men: significant increase in circulating estrogens. J Clin Endocrinol Metab. 1999;84(6):2170-2176. 17. Lewis GF, Alessi CA, Imperial JG, Refetoff S. Low serum free thyroxine index in ambulating elderly is due to a resetting of the threshold of thyrotropin feedback suppression. J Clin Endocrinol Metab. 1991;73(4):843-849. 18. Tahboub R. Thyroid dysfunction in the elderly. http://www.naama.com/pdf/thyroid-dysfunction-in-elderly-rund-tahboob-md.pdf. Accessed July 12, 2010. 19. Zeitzer JM, Daniels JE, Duffy JF, et al. Do plasma melatonin concentrations decline with age? Am J Med. 1999;107(5):422-436. 20. Sainz RM, Mayo JC, Tan DX, León J, Manchester L, Reiter RJ. Melatonin reduces prostate cancer cell growth leading to neuroendocrine differentiation via a receptor and PKA independent mechanism. Prostate. 2005;63(1):29-43. 21. Jung-Hynes B, Huang W, Reiter RJ, Ahmad N. Melatonin resynchronizes dysregulated circadian rhythm circuitry in human prostate cancer cells. J Pineal Res. 2010;49(1):60-68. 22. Srinivasan V, Spence DW, Pandi-Perumal SR, Trakht I, Cardinali DP. Therapeutic actions of melatonin in cancer: possible mechanisms. Integr Cancer Ther. 2008;7(3):189-203. 23. Carter HB, Pearson JD, Metter EJ, et al. Longitudinal evaluation of serum androgen levels in men with and without prostate cancer. Prostate. 1995;27(1):25-31.
Dan Carter, ND
Male hormone restoration implies that all hormones that decline with age or suboptimal metabolism should be restored to levels consistent with optimal physiologic function. Hormone restoration includes all major hormones that affect biologic function, including testosterone, dehydroepiandrosterone (DHEA), thyroid, and melatonin. Growth hormone is useful for many individuals as they age, but its expense eliminates it from consideration for most patients; hence, it will not be included in this discussion. What will be covered herein are some of the lesser-known benefits of hormone restoration, emphasizing testosterone.
Replacement:
1: the action or process of replacing: the state of being replaced.
2: one that replaces another especially in a job or function
Restoration: 1: an act of restoring or the condition of being restored: as a bringing back to a former position or condition. 2: something that is restored; especially: a representation or reconstruction of the original form
Merriam-Webster Online
When used in the context of improving a man’s health, hormone restoration is the better term. What happens during aging that can be related to hormone decline? Alterations include decreased capacity for cellular protein synthesis, decline in immune function, loss of muscle strength and function, fatigue, increased body fat, decreased bone density, erectile dysfunction, decreased libido, depressed mood, and more “age related” illness.1 These changes lead to age-related disability, including less strength and endurance, muscle atrophy, impaired mobility, less physical and mental energy, and osteoarthritis. The downward cycle resulting from these disabilities results in falls, fractures, loss of independence, and poor quality of life. Hormone restoration can delay the effects of aging and allow for a longer period in a functional and healthier state. This is an important aspect of preventive medicine.
Testosterone
The following quotation is from WebMD: “Testosterone levels decline steadily after age 40. The decline is relatively small, at an average rate of about 1% to 2% percent [sic] per year. By middle age and older, virtually all men experience some decline in testosterone — but only a small percentage of aging men have levels far below those considered normal for their age” (Hoffman M. Low testosterone explained: how do you know when levels are too low? http://men.webmd.com/features/low-testosterone-explained-how-do-you-know-when-levels-are-too-low). Table 1 gives androgen levels among subjects by age group. What the WebMD quotation implies is that testosterone should be adjusted to an age-normal level; more benefit is realized when testosterone is replaced to a level consistent with highest metabolic function (ie, the free testosterone level seen in the group aged 25-34 years). Blood testosterone is monitored by periodic serum concentration testing to ensure a safe and therapeutic level.
Risks and Contraindications of Testosterone Therapy
Histories of prostate cancer or breast cancer are absolute contraindications for testosterone therapy. Testosterone can make both of these hormone-sensitive cancers grow more rapidly. Possible Adverse Effects of Testosterone Therapy Following is a list of possible adverse effects of testosterone restoration:
1. Fluid retention. Some healthy older men have shown problems with fluid retention, leading to ankle or leg swelling, worse high blood pressure, and possibly congestive heart failure, according to older data. In a 2005 study of extracellular water in hypopituitary men, no patients reported adverse effects, and no clinical symptoms or signs associated with excess fluid retention were observed during treatment with the doses and regimen used for growth hormone, testosterone, or their combination.2
2. Liver toxic effects. To date, there are no reports of liver toxic effects from transdermal testosterone therapy. Oral testosterone therapy can cause significant liver problems.
3. Decreased fertility. Exogenous testosterone shuts down sperm production significantly or completely in almost all men, and this can be a temporary or permanent effect. It is recommended that men delay testosterone therapy until they have finished having children.
4. Sleep apnea. Increased testosterone levels may exacerbate preexisting sleep apnea. However, a 36-month trial of testosterone therapy in older men demonstrated no effect of treatment on apneic episodes.
5. Tender breasts and gynecomastia. This may occur in older men receiving testosterone therapy due to the conversion of testosterone to estrogen. Breast tissue is estrogen sensitive, and this adverse effect can be eliminated by decreasing the dosage or by prescribing an aromatase inhibitor.
6. Polycythemia. Men who develop polycythemia can lower their testosterone dosage or donate blood to decrease their blood cell mass. It is advisable to check hematocrit readings yearly.3 [Physicians commonly confuse malignant polycythemia vera with erythrocytosis. Testosterone increases erythropoeitin production by the kidneys. This is the same process that causes individuals who live at high altitudes to have increased red blood cell counts. Erythrocytosis does not need to be treated, as it is a benign condition].
7. Prostatic hyperplasia. Hyperplasia may be benign (benign prostatic hypertrophy), with its attendant problems with urination. Testosterone may promote the growth of cancerous prostate cells.
For carefully screened patients, the benefits of testosterone therapy are greater than the risks.
Low free testosterone levels are an independent risk factor for cardiovascular disease. Older men with low free testosterone levels and low high-density lipoprotein cholesterol concentrations showed more severe coronary artery blockage than those evaluated by predictors, including blood pressure, elevated cholesterol, diabetes mellitus, smoking, and body mass index.4
Possible Cardioprotective Activities of Testosterone Therapy
Testosterone exhibits a number of possible cardioprotective activities. Significant examples include the following:
• Reduces serum levels of the proinflammatory cytokines interleukin (IL) 1β and tumor necrosis factor
• Increases levels of the anti-inflammatory cytokine IL-10
• Reduces vascular cell adhesion molecule 1 expression in aortic endothelial cells
• Promotes vascular smooth muscle and endothelial cell proliferation
• Induces vasodilatation and improves vascular reactivity, to reduce serum levels of the prothrombotic factors plasminogen activator inhibitor 1 and fibrinogen
• Lowers low-density lipoprotein cholesterol concentrations
• Improves insulin sensitivity
• Reduces body mass index and visceral fat mass
Taken together, the actions of testosterone confer cardiovascular benefit, as testosterone therapy reduced atheroma formation in cholesterol-fed animal models and decreased myocardial ischemia in men with coronary heart disease.5 Insulin resistance occurs in chronic heart failure (CHF) and implies a worse prognosis.6 Investigations in men without CHF showed that physiologic testosterone therapy improves insulin sensitivity. This 2007 study6 showed that testosterone restoration improves fasting insulin sensitivity in men with CHF and increases lean body mass. The data suggest a beneficial effect of testosterone on an important metabolic component of CHF. Low testosterone levels predict cardiovascular events such as stroke and transient ischemic attack in older men and are associated with higher cardiovascular and overall mortality.7
Other Considerations Regarding Testosterone Therapy
Men with chronic medical or psychological illnesses should have their testosterone level measured, especially when sexual dysfunction symptoms or signs are present (eg, erectile dysfunction).8 Depression and hypogonadism are also associated with erectile dysfunction. Physicians should evaluate testosterone measurements in all men with high depression symptom scores.9 Metabolic syndrome and insulin resistance are also significantly associated with low testosterone levels in older men. Men with metabolic syndrome should not only have cardiovascular risks evaluated but also have testosterone levels assessed.10
Historically, visceral obesity, metabolic syndrome, diabetes mellitus, cardiovascular disease, and erectile dysfunction were viewed as independent conditions affecting the aging man. It is becoming recognized that hypogonadism is a common third denominator of a triad that includes erectile dysfunction and metabolic syndrome.11 Dehydroepiandrosterone
Dehydroepiandrosterone is the most common corticosteroid hormone in the body and is produced mainly by the adrenal glands. Dehydroepiandrosterone is derived from pregnenolone, which is metabolized from cholesterol. Dehydroepiandrosterone can be converted into other sex hormones, including testosterone and the estrogens, although this is more common in women.12 By age 60 years, DHEA levels are only about 5% to 15% of what they were at their peak at age 20 years and can be considered a biomarker of aging.13 Dehydroepiandrosterone has been reported to have beneficial effects for patients with diabetes, senile dementia, obesity, immunosuppression, and autoimmune conditions. It also shows promise in cancer prevention (by increasing natural killer cells), stress-induced diseases, aging, and heart disease.14,15
A suitable daily dose of dehydroepiandrosterone in aging men is 50 mg, as it leads to serum DHEA sulfate concentrations similar to those measured in young healthy adults.16 Serum testosterone and dihydrotestosterone levels remained unchanged after administration of 50 mg of dehydroepiandrosterone. However, 17-beta estradiol and estrone levels significantly increased to concentrations still within the upper normal range for men. A dehydroepiandrosterone-induced increase in estrogens may contribute to beneficial effects of DHEA in men.
Thyroid Hormone
Low free thyroid hormone levels can occur as a consequence of aging, despite normal thyrotropin levels.17 Certain prescription drugs can also effect total thyroxine (T4) metabolism, including carbamazepine, phenytoin, rifampin, and phenobarbital. Additional drugs such as amiodarone and lithium can affect thyroid function in other ways. Thyroid disease can also manifest with symptoms derived from the most diseased nonthyroid system in the patient.18 In the presence of normal thyrotropin values, patients with hypothyroid symptoms can benefit from having free T4 and total triiodothyronine values determined.
Melatonin
A common belief is that “melatonin levels slowly drop with age and older adults make very small amounts of it or none at all.” Older research supports the decrease in melatonin with aging, whereas newer research refutes it.19 Sleep disturbances become more common with aging, and sufficient restorative sleep is important for overall health. Melatonin also inhibits the growth of several types of cancer cells. Melatonin limits human prostate cancer cell growth by a mechanism that affects the regulation of androgen receptor function; other mechanisms may be involved.20,21 The physiologic surge of melatonin at night can be considered a “natural restraint” on tumor initiation, promotion, and progression.22 Although declining melatonin production during the aging process is not thoroughly elucidated, many patients experience better sleep with sufficient dosing. Melatonin dosage is based on the amount that gives restful sleep without morning grogginess.
Pre–Hormone Restoration Therapy Examinations
The following clinical and laboratory examinations should be considered a minimum workup before administering hormone restoration therapy:
• Complete blood cell count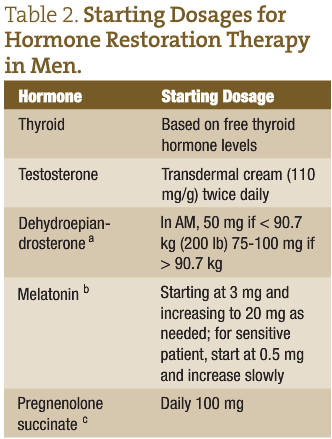
• Comprehensive metabolic panel
• Prostate-specific antigen test
• Digital rectal examination
• Testicular examination
A thorough medical history is also mandated.
Starting Dosages for Hormone Restoration Therapy
Table 2 gives starting dosages for hormone restoration therapy in men.
Testing of Hormone Levels
Hormone levels should be determined 1 month after initiation of hormone restoration therapy. Blood serum levels are the preferred testing method; blood should be drawn 5 hours after the morning dose of hormone. Testing applies to thyroid hormone, testosterone, and DHEA sulfate levels. Estradiol is not normally tested in men; the value is included for reference in Table 3. Melatonin level is not tested. Once a therapeutic hormone level is reached, testing is normally performed once a year. Optimal values are selected using the top end of the male normal range.
In conclusion, a carefully designed and monitored hormone restoration program improves the quality of life in aging men. For men exhibiting central obesity, often in conjunction with metabolic syndrome, it is important that they receive dietary counseling to help reduce visceral adiposity. Aromatase enzyme levels are increased in patients with visceral fat and high insulin levels; high aromatase levels convert too much testosterone to estrogen, leading to more abdominal and pectoral fat and gynecomastia. Visceral adiposity normally responds well to a diet that improves insulin sensitivity by restricting carbohydrate consumption, while supplying sufficient protein and fat.
Dan Carter, ND, graduated from National College of Naturopathic Medicine (NCNM) and completed a 2-year family practice resi-dency at the college. He was appointed to a full-time faculty position in 1997 and served as a core faculty member through 2003.He is a co-founder of IV Nutritional Therapy for Physicians, teaching intravenous thera-py workshops since 1991. These workshops provide com-plete training to physicians internationally for the safe and effective use of intravenous nutrient therapies. He has been in private practice in Bozeman, Montana since 2004. His practice focuses on the nutritional improvement of health, weight loss, hormone restoration for men and women, and IV nutrient therapy. Dr Carter’s websites can be accessed at www.alpinephysicians.com and www.bznwtmgt.com.
SIDEBAR • Meta-analysis indicates testosterone is not associated with increased risk of cancer • Testosterone does not cause cancer23 • Testosterone increases the growth of prostate cancer if present • Prostate cancer is most prevalent when testosterone levels are low
References 1. Winters SJ. Current status of testosterone replacement therapy in men. Arch Fam Med. 1999;8(3):257-263. 2. Johannsson G, Gibney J, Wolthers T, Leung KC, Ho KK. Independent and combined effects of testosterone and growth hormone on extracellular water in hypopituitary men. J Clin Endocrinol Metab. 2005;90(7):3989-3994. 3. Haijar R, Kaiser F, Morley J. Outcomes of long-term testosterone replacement in older hypogonadal males: a retrospective analysis. Clin Endocrinol Metab. 1997;82(11):3792-3796. 4. Phillips G, Pinkernell B, Jin T. Are major risk factors for mycocardial infarction the major predictors of degree of coronary artery disease in men? Metabolism. 2004;53(3):324-329. 5. Jones RD, Nettleship JE, Kapoor D, Jones HT, Channer KS. Testosterone and atherosclerosis in aging men: purported association and clinical implications. Am J Cardiovasc Drugs: 2005;5(3):141-154. 6. Malkin CJ, Jones TH, Channer KS. The effect of testosterone on insulin sensitivity in men with heart failure. Eur J Heart Fail. 2007;9(1):44-50. 7. Yeap B. Androgens and cardiovascular disease. Curr Opin Endocrinol Diabetes Obes. 2010;17(3):269-276. 8. Guay A, Seftel A, Traish A. Hypogonadism in men with erectile dysfunction may be related to a host of chronic diseases. Int J Impot Res. 2010;22(1):9-19. 9. Makhlouf, A, Mohamed, M, Seftel A, Niederberger C. Hypogonadism is associated with overt depression symptoms in men with erectile dysfunction. Int J Impot Res. 2008;20(2):157-161. 10. Guay A, Jacobson J. The relationship between testosterone levels, the metabolic syndrome (by two criteria), and insulin resistance in a population of men with organic erectile dysfunction. J Sex Med. 2007;4(4, pt 1):1046-1055. 11. Ahabsigh R. The triad of erectile dysfunction, hypogonadism and the metabolic syndrome. Int J Clin Pract. 2008;62(5):791-798. 12. Morales AJ, Nolan JJ, Nelson JC, Yen SS. Effects of replacement dose of dehydroepiandrosterone in men and women of advancing age [published correction appears in J Clin Endocrinol Metab. 1995;80(9):2799]. J Clin Endocrinol Metab. 1994;78(6):1360-1367. 13. Ebeling P, Koivisto VA. Physiological importance of dehydroepiandrosterone. Lancet. 1994;343(8911):1479-1481. 14. Rudman D, Shetty KR, Mattson DE. Plasma dehydroepiandrosterone sulfate in nursing home men. J Ann Geriatr Soc. 1990;38(4):421-427. 15. Kalimi M, Shafagoj Y, Loria R, Padgett D, Regelson W. Anti-glucocorticoid effects of dehydroepiandrosterone (DHEA). Mol Cell Biochem. 1994;131(2):99-104. 16. Arlt W, Haas J, Callies F, et al. Biotransformation of oral dehydroepiandrosterone in elderly men: significant increase in circulating estrogens. J Clin Endocrinol Metab. 1999;84(6):2170-2176. 17. Lewis GF, Alessi CA, Imperial JG, Refetoff S. Low serum free thyroxine index in ambulating elderly is due to a resetting of the threshold of thyrotropin feedback suppression. J Clin Endocrinol Metab. 1991;73(4):843-849. 18. Tahboub R. Thyroid dysfunction in the elderly. http://www.naama.com/pdf/thyroid-dysfunction-in-elderly-rund-tahboob-md.pdf. Accessed July 12, 2010. 19. Zeitzer JM, Daniels JE, Duffy JF, et al. Do plasma melatonin concentrations decline with age? Am J Med. 1999;107(5):422-436. 20. Sainz RM, Mayo JC, Tan DX, León J, Manchester L, Reiter RJ. Melatonin reduces prostate cancer cell growth leading to neuroendocrine differentiation via a receptor and PKA independent mechanism. Prostate. 2005;63(1):29-43. 21. Jung-Hynes B, Huang W, Reiter RJ, Ahmad N. Melatonin resynchronizes dysregulated circadian rhythm circuitry in human prostate cancer cells. J Pineal Res. 2010;49(1):60-68. 22. Srinivasan V, Spence DW, Pandi-Perumal SR, Trakht I, Cardinali DP. Therapeutic actions of melatonin in cancer: possible mechanisms. Integr Cancer Ther. 2008;7(3):189-203. 23. Carter HB, Pearson JD, Metter EJ, et al. Longitudinal evaluation of serum androgen levels in men with and without prostate cancer. Prostate. 1995;27(1):25-31.
It is a long established fact that a reader will be distracted by the readable content of a page when looking at its layout. The point of using Lorem Ipsum is that it has a more-or-less normal distribution of letters, as opposed to using ‘Content here, content here’, making it look like readable English. Many desktop publishing packages and web page editors now use Lorem Ipsum as their default model text, and a search for ‘lorem ipsum’ will uncover many web sites still in their infancy.
It is a long established fact that a reader will be distracted by the readable content of a page when looking at its layout. The point of using Lorem Ipsum is that it has a more-or-less normal distribution of letters, as opposed to using ‘Content here, content here’, making it look like readable English. Many desktop publishing packages and web page editors now use Lorem Ipsum as their default model text, and a search for ‘lorem ipsum’ will uncover many web sites still in their infancy.
The point of using Lorem Ipsum is that it has a more-or-less normal distribution of letters, as opposed to using ‘Content here, content here’, making

The point of using Lorem Ipsum is that it has a more-or-less normal distribution of letters, as opposed to using ‘Content here, content here’, making it look like readable English. Many desktop publishing packages and web page editors now use Lorem Ipsum as their default model text, and a search for ‘lorem ipsum’ will uncover many web sites still in their infancy.
It is a long established fact that a reader will be distracted by the readable content of a page when looking at its layout. The point of using Lorem Ipsum is that it has a more-or-less normal distribution
Copyright BlazeThemes. 2023